Epidemiology and health intelligence
Better, more sustainable, and locally responsive population health intelligence systems are needed to monitor non-communicable diseases (NCDs), their impacts on population health, and the response of health and care systems.
Research in this theme critically investigates the sharing and collaborative use (and limits) of national and local electronic healthcare record/registry (EHR) data and their linkages as sources of data and intelligence for population health management. This includes conducting large-scale population surveys and, with participant consent, linking patient-reported measures to EHR data to estimate the distribution of NCDs, and associated disability, health-related quality of life, and employment outcomes, as well as patterns of healthcare utilization. A feature of many ‘forgotten’ NCDs is the relative absence of population health metrics and tools to support evaluation and predictive prevention. We work with academic and non-academic partners to develop, evaluate, and implement new measures and tools to address these gaps.
Estimating Healthy Working Life Expectancy in England
Healthy working life expectancy (HWLE) is a population indicator that takes account of both health and work states and provides an indication of whether extensions to working life are achievable. This work is increasingly valued by the Department for Work and Pensions (DWP) who are interested in:
- the estimates of HWLE to inform pension policy,
- the identification of factors and mechanisms that are amenable to change and could be targeted by health and social policy to increase the number of years people remain healthy and in work. The range of potentially modifiable health and social targets will require a number of approaches; a social approach to reduce the impact of social, psychological and lifestyle factors, and a policy approach to address inequities to care and interventions in the workplace.
The HWLE team are developing methods for calculating HWLE on a continuous basis as a measure of long term trends in workability of older adults. The team collaborate with the Joint Work and Health Unit within DWP and the Fuller Working Lives/State Pension Age group who are interested in the results linked to the role of the employer and workplace adjustment on HWLE.
Links: Centre for Musculoskeletal Health & Work, HLWE
People: Marty Parker, Ross Wilkie, Milissa Bucknall
Key references:
- Population-based estimates of healthy working life expectancy in England at age 50 years: analysis of data from the English Longitudinal Study of Ageing. Lancet Public Health. 2020.
- Extending Working Lives: A Systematic Review of Healthy Working Life Expectancy at Age 50. Soc Ind Res. 2020
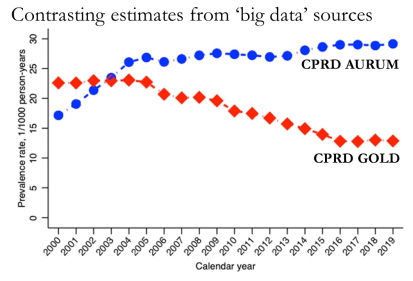
Defining non-communicable diseases and quality of care in the electronic health record
Electronic health records, created in the process of providing care, are a potentially powerful source of information for monitoring health and care in populations. Research on how to define non-communicable diseases, care processes, determinants, and outcomes within the electronic health record underpins their valid and meaningful re-use for population health management.
|
Links: MRR People: Kelvin Jordan, Dahai Yu, John Edwards, Krysia Dziedzic Key references:
|
Musculoskeletal Health Questionnaire (MSK-HQ)
Musculoskeletal outcome tools are fragmented across different settings and conditions. Working with colleagues in the University of Oxford and with Versus Arthritis, this research aimed to provide patients and practitioners across the musculoskeletal pathway with a practical tool for quantifying and monitoring the impact of musculoskeletal symptoms.
- Development of the new measure and evaluation of its measurement properties
- Exploring how managerial and commissioning decisions are influenced by the availability of MSK-HQ outcome data
- Implementation in local musculoskeletal services
Links: MSK-HQ, MSK-Tracker
People: Dr Jonathan Hill
Key references:
- Development and initial cohort validation of the Arthritis Research UK Musculoskeletal Health Questionnaire (MSK-HQ) for use across musculoskeletal care pathways. BMJ Open. 2016.
- Determining responsiveness and meaningful changes for the Musculoskeletal Health Questionnaire (MSK-HQ) for use across musculoskeletal care pathways. BMJ Open. 2019.
Trends, projections, and variation in health and healthcare
Which health problems are becoming more common? How have patterns of care been changing? What evidence is there for significant variation in these and what seems to determine this? What about health and care in special populations, such as children and adolescents? What future rates and patterns we should be planning for? Our descriptive studies use a range of population data sources at local, national, and international levels to provide some answers and inform future research and action to improve health and reduce health inequalities.
Musculoskeletal health and care
People: Kelvin Jordan, Dahai Yu, Sara Muller, Kate Dunn
Key references:
- Incidence, prevalence and treatment burden of polymyalgia rheumatica in the UK over two decades: a population-based study. Ann Rheum Dis 2018.
- Trends in the prevalence, incidence and surgical management of carpal tunnel syndrome between 1993 and 2013: an observational analysis of UK primary care records. BMJ Open 2018.
- Population trends in the incidence and initial management of osteoarthritis: age-period-cohort analysis of the Clinical Practice Research Datalink, 1992-2013. Rheumatology, 2017.
- Musculoskeletal consultations from childhood to adulthood: a longitudinal study. J Public Health 2019.

|
Fitnotes and sickness absencePeople: Gwen Wynne-Jones, Ross Wilkie
|
Opioids and other dependence-forming prescription medicines
People: Christian Mallen, Kate Dunn, Julie Ashworth
Key references:
- Trends in gabapentinoid prescribing in patients with osteoarthritis: a United Kingdom national cohort study in primary care. Osteoarthritis Cartilage 2019.
- Risk of adverse events in patients prescribed long-term opioids: A cohort study in the UK Clinical Practice Research Datalink. Eur J Pain 2019.
- Increased risk of reproductive dysfunction in women prescribed long-term opioids for musculoskeletal pain: A matched cohort study in the Clinical Practice Research Datalink. Eur J Pain 2018.
- Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med 2010.
Cardiovascular health and care
People: Mamas Mamas
Key references:
- Socioeconomic status and differences in the management and outcomes of 6.6 million US patients with acute myocardial infarction. Am J Cardiol 2020.
- 20-year trend in cause-specific heart failure outcomes by sex, socioeconomic status, and place of diagnosis: a population-based study. Lancet 2019.
- Multimorbidity and survival for patients with acute myocardial infarction in England and Wales: Latent class analysis of a nationwide population-based cohort. BMC Medicine 2018.
- Explaining North-South disparities in mortality rates among 25-44 year olds in England: a longitudinal population study. Lancet Public Health 2018.
- Geographical epidemiology of health and overall deprivation in England, its changes and persistence from 2004 to 2015: a longitudinal spatial population study. J Epidemiol Comm Health 2018.
Mental health and care
People: Carolyn Chew-Graham, Kelvin Jordan
Key references:
- Incidence, clinical management, and mortality risk following self harm among children and adolescents: cohort study in primary care. BMJ 2017.
Population health intelligence and predictive prevention
Modelling linked survey and electronic health record data for sustainable population health indicators (PRELIM / HILL)
|
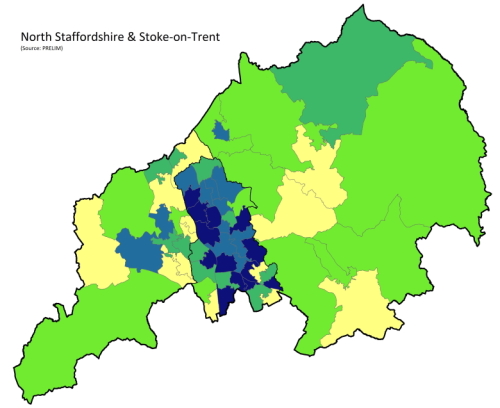
PRELIM The PRELIM initiative aims to provide a detailed description of musculoskeletal health, key comorbidity and care among consulters and the general population by linking a musculoskeletal-focused patient survey to local, high-quality, primary care electronic health record data using robust epidemiological approaches. The purpose is to contribute to a system of musculoskeletal health intelligence in the UK population that provides useful, timely, sustainable, trustworthy evidence for policymakers, practitioners, and the public. People: Ross Wilkie, Dahai Yu, Kelvin Jordan, George Peat |
Health Intelligence in the West Midlands study (the Hill study)
The Health Intelligence in the West Midlands study (Hill study) was designed to provide new evidence and insights to underpin and inform the prevention and management of non-communicable diseases that cause the greatest burden in years lived with disability in the United Kingdom. The study will examine the extent of health inequalities in the impact of non-communicable diseases and identify the key social and behavioural risk factors that determine them. A series of ‘Spotlight Studies’ will offer local doctors, allied health professionals and nurses in training a range of supervised research projects, based on local health data, in key areas of importance and supervisory expertise.
Enriched data integration for population musculoskeletal health intelligence (MIDAS)
Reducing the burden of common musculoskeletal (MSK) conditions requires better integration of data upstream of hospital care, however, meaningful data collected from surveys, primary care records and community service providers have not so far been linked together. This project seeks to overcome these barriers by developing a novel and scalable approach within North Staffordshire & Stoke-on-Trent.
Links: Read the full project overview on the Nuffield Foundation website.
People: George Peat, Kelvin Jordan, Krysia Dziedzic, Ross Wilkie, Jonathan Hill
Prediction models and individual risk prediction
Individual risk prediction is one of the fundamental ‘uses of epidemiology’ and can underpin better information for individuals and practitioners and targeting of resources within populations for earlier treatment and prevention. Working closely with our Centre for Prognosis Research, we use a variety of ‘big data’ sources to develop, validate, and evaluate a range of risk prediction models.
Links: Centre for Prognosis Research
People: Richard Riley, Kelvin Jordan, Kym Snell, Joie Ensor, Dahai Yu
Key references:
- External validation of clinical prediction models using big datasets from e-health records or IPD meta-analysis: opportunities and challenges. BMJ 2016.
- Patterns of symptoms before a diagnosis of first-episode psychosis: a latent class analysis of UK primary care electronic health records. BMC Med 2019.
- Development and validation of prediction models to estimate risk of primary total hip and knee replacements using data from the UK: two prospective open cohorts using the UK Clinical Practice Research Datalink. Ann Rheum Dis 2018.
- Prognosis of undiagnosed chest pain: linked electronic health record cohort study. BMJ 2017.


