| Chief Investigator: | Professor Kelvin Jordan |
| Principal Investigators: | Dr Michelle Marshall / Dr Paul Campbell |
| Funder name / reference number: | Dunhill Medical Trust (RPGF 1711/11) |
| Year: | 2018-2020 |
Study Team:
Michelle Marshall1, Paul Campbell1,2, Trishna Rathod-Mistry1, James Bailey1, Carolyn Chew-Graham1,2, Martin Frisher1, Richard Hayward1, Rashi Negi2, Louise Robinson3, Swaran Singh4, Athula Sumathipala1,2, Nwe Thein2, Kate Walters5, Scott Weich6, Kelvin Jordan1
1Keele University, 2Midlands Partnership NHS Foundation Trust, 3Newcastle University, 4University of Warwick, 5University College London, 6University of Sheffield
Video
Click below to watch our video on this study. You can also visit our dissemination tab to view an animation that summarises MEDDIP and its findings.
The number of people living with dementia is increasing. Previous research has looked at what factors increase the risk of dementia, but less is known about how dementia affects people over time once they have been diagnosed.
Most healthcare for dementia is provided by general practitioners and practice nurses. One of the quickest ways to identify common patterns of the course of dementia after diagnosis may be to use existing medical records from primary care. Having the ability to look at the course of dementia over time in these records will help identify people who have a poorer progression and also identify the factors that may be related to this poorer progression.
The aim of the MEDDIP study was to test whether we can identify markers of dementia progression, and identify common patterns of progression, using information stored in primary care medical records. There were 3 stages to the study:
Stage 1
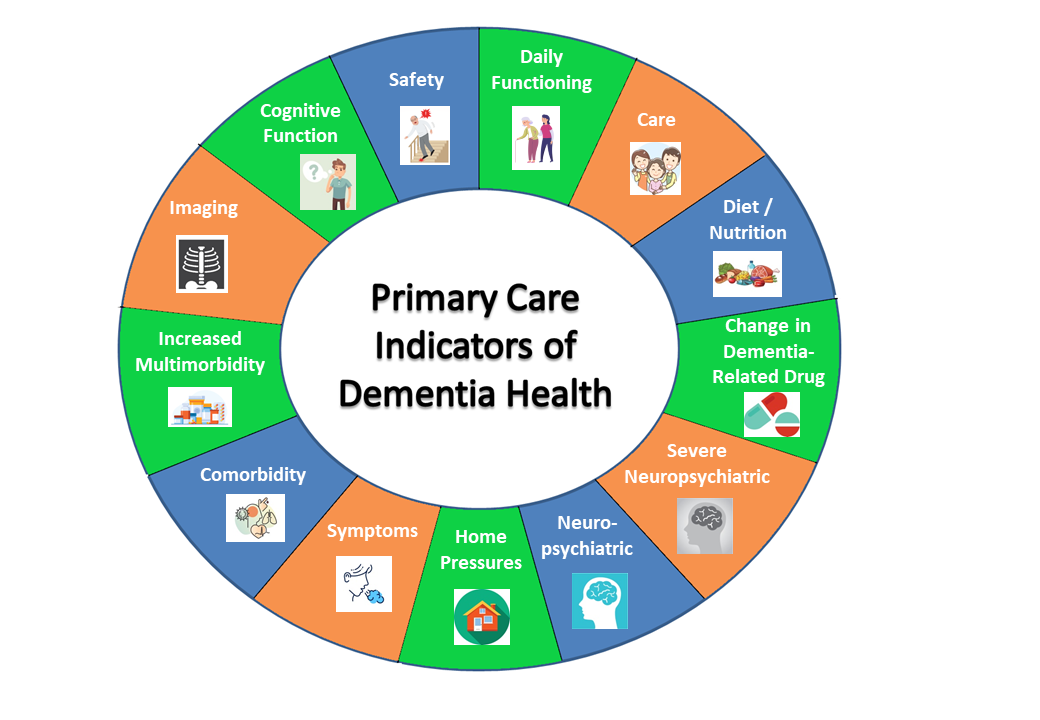
Through i) a review of previous studies, ii) discussions with health professionals, researchers, people with dementia and their care givers, and iii) analysis of a small primary care medical record database, we identified possible markers of progression that can be identified from medical records and are related to dementia. These were grouped into 13 domains.
Stage 2
In a linked study (the CoMed study), we assessed how well these potential markers of dementia progression are associated with changes in the course of the condition as recorded at a specialist dementia service.
Stage 3
We used a large UK-wide primary care medical record database containing records of over 30,000 patients with dementia to find out if these markers are related to longer-term outcomes such as being admitted to hospital and dying earlier.
Impact
We have identified markers of dementia progression that are recorded in primary care, and grouped them into domains. These may help identify individuals who are at risk of a poorer long-term course of their dementia, and hence may benefit from more targeted treatment and care. Some markers are modifiable and targeting these may also help alter the course of someone’s illness. Future research studies may also be able to assess progression and outcomes using these markers, hence potentially saving time and reducing costs of research.
This figure shows the 13 domains of markers of dementia progression that are identifiable in primary care medical records.
Please click here to download a copy of the full figure of domains and associated markers.
An animation and a talking heads video have been produced summarising the MEDDIP and its findings:
Publications
Journal articles:
Campbell P, Rathod-Mistry T, Marshall M, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Singh S, Tantalo-Baker S, Tarafdar S, Babatunde OO, Robinson L, Sumathipala A, Thein N, Walters K, Weich S, Jordan KP. (2020) Markers of dementia-related health in primary care electronic health records. Aging & Mental Health, 1-11. DOI: 10.1080/13607863.2020.1783511
PubMed: https://pubmed.ncbi.nlm.nih.gov/32578454/
Full text: https://www.tandfonline.com/doi/pdf/10.1080/13607863.2020.1783511
Rathod-Mistry T, Marshall M, Campbell P, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Robinson L, Singh S, Sumathipala A, Thein N, Walters K, Weich S, Jordan KP. (2020) Indicators of dementia disease progression in primary care: an electronic health record cohort study. European Journal of Neurology, 1-28. DOI:10.1111/ene.14710
PubMed: https://pubmed.ncbi.nlm.nih.gov/33378599/
Full text: https://doi.org/10.1111/ene.14710
Marshall M, Campbell P, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Rathod-Mistry T, Singh S, Robinson L, Sumathipala A, Thein N, Walters K, Weich S, Jordan KP. (2022) Feasibility of linking markers of dementia-related health in primary care medical records to cognitive function assessed in a specialist dementia service. medRxiv, DOI: 10.1101/2022.10.11.22279756
Full text: https://doi.org/10.1101/2022.10.11.22279756
Conference abstracts:
- Rathod-Mistry T, Marshall M, Campbell P, Bailey J, Chew-Graham CA, Frisher M, Hayward R, Negi R, Singh S, Sumathipala A, Thein N, Walters K, Weich S. (2020) Can early markers of poor long-term outcomes in dementia be identified from primary care electronic health records? Society for Academic Primary Care Annual Scientific Meeting 2020. >>link
- Campbell P, Rathod-Mistry T, Marshall M, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Singh S, Sumathipala, Thein N, Walters K, Weich S, Jordan KP. Can markers of dementia progression be derived from primary care electronic health records? Society for Academic Primary Care Annual Scientific Meeting 2019, Exeter, UK. >>link (Page 166).
- Campbell P, Baker S, Tarafdar S, Babatunde O, Croft P, Chew-Graham CA, Robinson L, Walters K, Singh S, Weich S, Jordan KP. Can markers of dementia progression and outcomes be derived from electronic health records? A systematic review. Society for Academic Primary Care Annual Scientific Meeting 2019, Exeter, UK. >>link (Page 150).
- Campbell P, Baker S, Tarafdar S, Babatunde O, Croft P, Chew-Graham CA, Robinson L, Walters K, Singh S, Weich S, Jordan KP. Markers of dementia progression and outcomes in electronic health records: a systematic review. Health Services Research UK Conference 2019, Manchester, UK.
- Marshall M, Campbell P, Rathod-MistryT, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Robinson L, Singh S, Sumathipala A, Thein N, Walters K, Weich S, Jordan K. (2020) Can markers of dementia progression be derived from primary care electronic health records? 34th Virtual International Conference of Alzheimer’s Disease International – Poster Presentation.
- Marshall M, Campbell P, Rathod-MistryT, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Robinson L, Singh S, Sumathipala A, Thein N, Walters K, Weich S, Jordan K. (2021) Validating primary care markers of the course of dementia through linkage to secondary care records. Society for Academic Primary Care Annual Scientific Meeting 2021 - Oral presentation
- Marshall M, Campbell P, Rathod-MistryT, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Negi R, Robinson L, Singh S, Sumathipala A, Thein N, Walters K, Weich S, Jordan K. (2021) Primary care markers of the course of dementia: validation through linkage to cognitive function recorded in secondary care records. Primary Care Mental Health Research Conference - Oral presentation
- Negi R, Marshall M, Campbell P, Rathod-Mistry T, Bailey J, Chew-Graham CA, Croft P, Frisher M, Hayward R, Robinson L, Singh S, Sumathipala A, Thein N, Walters K, Weich S, Jordan K. (2021) Can markers of Dementia-related health be derived from primary care electronic health records? Royal Society of Psychiatry Faculty of Old Age Annual Conference - Poster presentation.
Contact Information:
Principal Investigator: Dr Michelle Marshall m.marshall@keele.ac.uk
Chief Investigator: Professor Kelvin Jordan k.p.jordan@keele.ac.uk