STOPS+
Supervised treatment in outpatients for schizophrenia plus (STOPS+): protocol for a cluster randomised trial of a community-based intervention to improve treatment adherence and reduce the treatment gap for schizophrenia in Pakistan.
This project is led by colleagues in the Institute for Global Health.
Schizophrenia is a severe long-term mental health condition. It causes a range of different psychological symptoms including hallucinations (hearing or seeing things that don't exist), delusions (unusual beliefs not based on reality), muddled thoughts based on hallucinations or delusions and changes in behaviour. Schizophrenia is a common cause of long-term disability in the 15-49-year-old group and whilst effective treatments are available, in developing countries around two-thirds of patients receive no treatment.
This lack of treatment, commonly known as the 'treatment gap' arises due to factors including poor treatment adherence, a lack of primary care involvement and poor access treatments. We have previously reported a new approach (Supervised Treatment in Out-Patients for Schizophrenia (STOPS)) that resulted in improved treatment adherence and functioning in a resource-poor setting in Khyber Pakhtunkhwa (KP), Pakistan. In this study we trained and supported relatives and family members to monitor medication taking, building on the success of a similar approach used for patients with tuberculosis.
We now aim to implement and evaluate a 'scaled-up' version of STOPS (STOPS+) which is based on the World Health Organisation mental health guidelines and maintain treatment adherence with the help of family members and text message reminders. We will work with primary care physicians and multipurpose primary are technicians to task shift care, under the supervision of mental health experts.
STOPS+ has 3 phases:
Phase 1: pre-implementation phase
Involving community engagement, modification of STOP to STOPS+ (involving patient, healthcare and wider community partners) and the identification of potential study participants.
Phase 2: implementation of STOPS+ in primary care settings using a cluster trial design
To determine the clinical and cost-effectiveness. 24 primary care centres in district Peshawar, KP will be randomised to deliver either STOPS+ or Enhanced Treatment As Usual (ETAU). We will recruit 526 patients (263 in each arm) suffering from Schizophrenia or schizoaffective disorder based on the International Classification of Diseases (ICD)-10 criteria. The outcomes of interest will include Global Assessment of Functioning and adherence to treatment regimen.
Phase 3: evaluation of the implementation in real world setting
This will be measured using the standardised World Health Organization's Assessment Instrument for Mental Health Systems (WHO-AIMS), economic evaluation, secondary data from the trial and utilisation of primary health care, and in-depth interview study involving all participants.
If successful this trial will improve schizophrenia care, improving lives for patients and their families. This work will provide important information for policymakers and set the foundations for reducing disability and improving long term patient outcomes.
STOPS+ is led by Professor Saeed Farooq, with Keele Co-Investigators Professor Lisa Dikomitis, Professor Christian Mallen, Professor Krysia Dziedzic, Dr Martyn Lewis and Dr Tom Shepherd and a team of researchers in Pakistan at the Khyber Medical University.

|

|

|

|

|

|

|
|
|
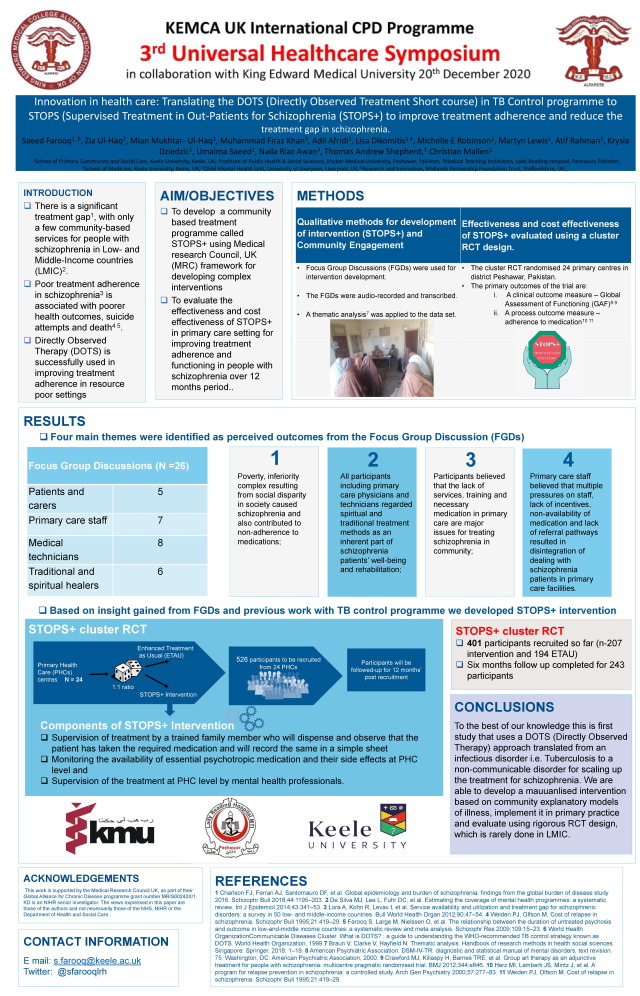
The STOPS+ research team won the second prize in KEMCAUK (King Edward Medical College Alumni Association of UK) in the Universal Healthcare Symposium (December 2020):
Published STOPS+ protocol in BMJ Open can be found online.
Alternatively, you can download the PDF version of the STOPS+ protocol below:
This file may not be suitable for some users of assistive technology
Request an accessible format



















