Centre for Regenerative Medicine Research
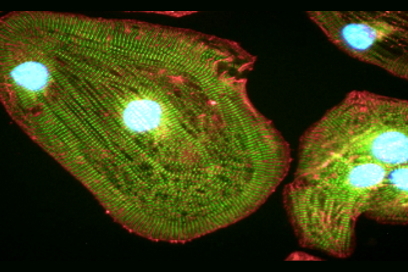
Keele University has an exceptional track record in bench and bed-side Regenerative Medicine research, which is recognised across the University and in the wider national and international academic and clinical communities.
The Centre for Regenerative Medicine Research strives to build on Keele’s internal and external reputation in this research space. Key to the success of this, as our long-term vision, is the cultivation of cross-School/University-wide collaborations, improving clinical and industrial engagement and supporting our members, in particular our outstanding early career researchers.
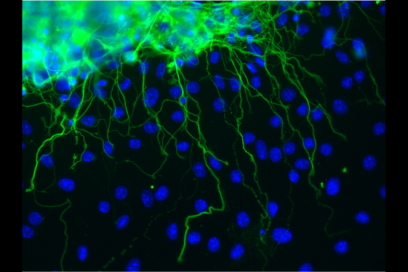
- Dr Heidi Fuller and Dr Monte Gates have secured a Leverhulme Trust grant worth £118k to investigate “What makes two overlapping groups of dopamine neurons so different?”
- ICRS Focus Meeting Allografts & Synthetics Scholarship awarded to Dr Jade Perry. ECMage Exchange and Mobility Funding awarded to Dr Oksana Kehoe, which will allow HenryBarrett (PhD Student) to visit their collaborators at the King's College London, Guy’s Hospital to lean the technique of regulatory T cells expansion.
- Dr Karina Wright and Prof Snow are Key Researchers in the Next Generation Therapies Theme of the Birmingham NIHR Biomedical Research Centre Renewal. As part of this collaboration the Oswestry team have been awarded funding for a 5-year Technical Post. Please click here for further details.
Davies R, Allen S, Mennan C, Platt M, Wright K, Kehoe O. Extracellular vesicle depletion protocols of foetal bovine serum influence umbilical cord mesenchymal stromal cell phenotype, immunomodulation, and particle release (2023). Int J Mol Sci. In Press.
Wilkinson, H., McCarthy, H. S., Perry, J., Smith, T., Wright, K., & Cool, P. Genomic Sequencing to Diagnose Prosthetic Joint Infection in the Knee: A Case Report (2023). Cureus, doi.org/10.7759/cureus.38788.
Hulme C, Mennan C, McCarthy H, Davies R, Lan T, Rix L, Perry J, Wright KT. A Comprehensive Review of Quantum Bioreactor Cell Manufacture: Research and Clinical Applications (2023) Cytotherapy. In Press.
Hulme CH, Peffers MJ, Roberts S, Gallacher P, Jermin P & Wright K. (2023). Proteomic Analyses of Autologous Chondrocyte Implantation Plasma Highlight Cartilage Acidic Protein 1 as a Candidate for Preclinical Screening. American Journal of Sports Medicine, In Press.
McCarthy HS, Tins B, Gallacher PD, et al. (2023). Histological and Radiological Assessment of Endogenously Generated Repair Tissue In Vivo Following a Chondral Harvest. CARTILAGE. 2023;0(0). doi:10.1177/19476035221149523
Harrison P, Hopkins T, Hulme C, McCarthy HS, Wright K. (2023). Chondrocyte Isolation and Expansion. In: Stoddart, M.J., Della Bella, E., Armiento, A.R. (eds) Cartilage Tissue Engineering. Methods in Molecular Biology, vol 2598. Humana, New York, NY. doi.org/10.1007/978-1-0716- 2839-3_2
Snow M, Kuiper JH, James S, Keeling E, Rich S, Amit P. (2023). A pilot randomised controlled trial assessing standard versus dermal patch-augmented rotator cuff repair found no adverse effects and suggest future trials need a minimum of 150 patients. Knee Surg Sports Traumatol Arthrosc. 2023 Mar 2. doi:10.1007/s00167-023-07356-5.
Snow M, Middleton L, Mehta S, Roberts A, Gray R, Richardson J, Kuiper JH, et al. (2023) ACTIVE Consortium A Randomized Trial of Autologous Chondrocyte Implantation Versus Alternative Forms of Surgical Cartilage Management in Patients With a Failed Primary Treatment for Chondral or Osteochondral Defects in the Knee. Am J Sports Med. Feb;51(2):367-378. doi:10.1177/03635465221141907.
Makos A, Kuiper JH, Kehoe O, Amarasena R. Psoriatic arthritis: review of potential biomarkers predicting response to TNF inhibitors. Inflammopharmacology. 2023 Feb;31(1):77-87. doi: 10.1007/s10787-022-01092-x. Epub 2022 Dec 12. PMID: 36508130; PMCID: PMC9957889.